 Deriving usable energy from dietary fats, carbohydrates, and amino acids involves a multitude of complex chemical reactions. Likewise, using dietary components to build and maintain our bodies also requires us to modify and process these molecules. To accomplish this we use enzymes, and for enzymes to function efficiently they often need cofactors in the form of vitamins and minerals.
Deriving usable energy from dietary fats, carbohydrates, and amino acids involves a multitude of complex chemical reactions. Likewise, using dietary components to build and maintain our bodies also requires us to modify and process these molecules. To accomplish this we use enzymes, and for enzymes to function efficiently they often need cofactors in the form of vitamins and minerals.
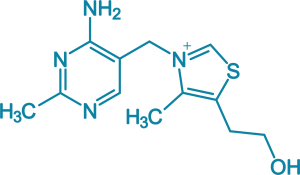
Dietary thiamine performs this cofactor function, but first it must be processed and “activated” by phosphorylation inside cells to thiamine pyrophosphate and other phosphate esters.This activation is driven by the enzyme thiamine pyrophosphokinase, which in turn requires magnesium and ATP bound together as a complex. Other phosphate esters also include thiamine monophosphate and thiamine triphosphate.
Once activated, thiamine pyrophosphate may be used as a cofactor for a range of enzymes involved in energy metabolism. As the cofactor for an enzyme complex called pyruvate dehydrogenase, thiamine is essential for how the body derives energy from glucose in the Krebs cycle.
Another thiamine-dependent Krebs cycle enzyme complex is alpha-ketoglutarate dehydrogenase. Located in the mitochondria of the cell, this enzyme is involved in the processing of both glucose and fats for energy, as well as processing amino acids and neurotransmitters.
Insufficient thiamine can downregulate these enzymes [1, 2] and therefore reduce the rate at which cells are able to synthesize energy. A more recent discovery has shown that thiamine is necessary for the alpha-oxidation of phytanic acid and 2- hydroxy straight-chain fatty acids, through the action of an enzyme called HACL-1 & 2 [3].
Dietary proteins are broken down into amino acids, and one class of amino acids is the branched-chain amino acids (valine, leucine, and isoleucine). The thiamine-dependent enzyme, branched-chain-keto acid dehydrogenase, is required to process and make use of these specific amino acids. In fact, without this enzyme the amino acids can accumulate at toxic levels, which is seen in the inherited genetic condition Maple syrup Urine Disease [4] .
Furthermore, utilizing glucose for anabolic (building) reactions in the pentose-phosphate pathway depends on the transketolase enzyme, which also requires both thiamine and magnesium cofactors. This pathway is needed to synthesize the building blocks of DNA, fatty acids, and in regenerating our primary intracellular antioxidant glutathione, amongst many other things. Without sufficient thiamine, the activity of transketolase is reduced and these crucial functions are downregulated [5].
The activity of other enzymes are also influenced by thiamine phosphate esters, where thiamine is not acting as a cofactor but is instead involved in:
- Allosteric regulation of pyridoxal kinase (enzyme involved in vitamin B6 activation) [6]
- Allosteric activation of glutamate dehydrogenase (one enzyme responsible for glutamate clearance to reduce neuroexcitoxicity) [6,7]
- Allosteric activation of malate dehydrogenase (a mitochondrial enzyme involved in ATP synthesis) [6]
Brain & Nervous System
Thiamine is especially important in the brain and central nervous system. Due to its role in the pentose phosphate pathway, it is expected that deficiency would result in decreased fatty acid synthesis required to maintain myelin sheath [8]. Indeed, demyelination of neurons is a known consequence of severe thiamine deficiency [9].
Thiamine is also required to maintain sufficient levels of the neurotransmitter acetylcholine in the brain [10, 11] The balance between the excitatory and inhibitory neurotransmitters GABA and glutamate is governed partially by thiamine-dependent enzymes, and deficiency can induce neuroexcitotoxicity [12]. Some research indicates that different forms of thiamine also play non-cofactor roles such as maintaining neuronal ion channels [13] and facilitating synaptic release of neurotransmitters including dopamine [14].
Because of their high demand for energy, certain areas of the “lower” regions of the brain are particularly susceptible to thiamine deficiency. This includes the mamillary bodies, thalamus, hypothalamus, brain stem, and cerebellum [15]. Aside from many other functions, these regions are responsible for coordinating the activity of the autonomic nervous system. This system is tasked with controlling all of the involuntary bodily processes including blood pressure, heart rate, blood vessel dilation and constriction, body temperature and digestion. When these brain regions lack thiamine, they can no longer generate energy efficiently. An energy deficit in these regions may therefore lead to a malfunctioning system [16]. The resulting autonomic dysfunction can have myriad downstream consequences on the other organs bodily systems – including the gastrointestinal and cardiovascular apparatus.
Insufficiency
The most well-known disease caused by nutritional thiamine deficiency is Beriberi. Originally identified in Japan, this condition is known to manifest primarily as neurological, cardiovascular, and/or gastrointestinal dysfunction. In some cases a severe thiamine deficiency may produce Wernicke’s Encephalopathy and/or Korsakoff’s Syndrome, both of which involve degenerative changes in the brain.
Although the above conditions are now considered rare in developed nations, mild to severe insufficiencies of thiamine may be much more prevalent than was once previously thought. Chronic consumption of energy-dense processed foods bereft of essential micronutrients increases the likelihood of vitamin and mineral deficiencies. And due to thiamine’s essential role in processing of glucose for energy, a diet high in refined carbohydrates will almost certainly have a detrimental impact on the body’s thiamine status [17].
Below is a brief list of the main establish causes of thiamine deficiency:
- Chronic alcohol consumption
- High intake of refined carbohydrate/sugar intake and processed macronutrients
- Chronic digestive issues involving malabsorption, inflammatory bowel diseases and gastric surgery
- Excessive intake of thiamine antagonists:
- Medications such as metformin
- Tannins in tea and coffee
- Thiamine-degrading enzymes (thiaminases) found in raw fish
- Long-term use of certain medications such as loop diuretics
Issues with ordinary thiamine supplements
The most common forms of thiamine found in nutritional supplements are thiamine salts (hydrochloride & mononitrate). However, the intestinal transport system is saturable, meaning that absorption/bioavailability hits a ceiling and is estimated to be low at approximately 3-10%. To achieve great increases in blood thiamine concentrations, high doses must be taken.
Furthermore, transport of free thiamine across the blood brain barrier is thought to be a slow process [18], and so thiamine salts are unable to significantly increase thiamine levels in the brain as well as other formulations can.
Finally, the transport of thiamine into cells is dependent on membrane rate-limiting transport proteins which are also saturable. There are also a variety of genetic polymorphisms which may predispose to less efficient cellular absorption and utilization [19].
With the above factors taken into consideration, it is important to choose a form of thiamine which can bypass these potential difficulties. And here is where TTFD comes in.
TTFD – Thiamine Tetrahydrofurfuryl Disulfide
Thiamine tetrahydrofurfuryl disulfide (TTFD) is one of several thiamine derivatives originally synthesized and studied extensively in Japan. The molecular configuration of TTFD closely resembles a specific form of thiamine found in garlic, known as allithiamine. TTFD is synthesized by attaching an organosulfur group (a mercaptan) to the chemical structure of the thiamine molecule.
The disulfide portion of TTFD allows thiamine to freely diffuse across membranes without the requirement for a transport protein. The rate-limiting transport system can therefore be bypassed both at the intestinal and the cellular level. Due to this quality, TTFD produces high levels of thiamine in the cell to be utilized for biochemical reactions, and the intestinal bioavailability is much greater than thiamine salts [20].
It is water-soluble, although due to its capacity to transit through the lipid bilayer of cell membranes it is often referred to as “lipid-soluble”. TTFD has been shown to increase organ thiamine content to a greater degree than thiamine salts [21], and may also possess antioxidant [22] & anti-inflammatory properties [23]. It has been shown to be non-toxic, even at high levels.
Furthermore, TTFD crosses the blood-brain-barrier and rapidly saturates brain cells with thiamine [24], which makes it a superior alternative to other forms of thiamines for restoring levels in the brain and central nervous system.
The most well-known proponent of TTFD is consultant paediatrician Dr Derrick Lonsdale, who pioneered the use of this molecule in clinical practice [25]. Lonsdale obtained licences to study TTFD extensively over many years, and has since authored multiple books, articles, and academic research papers on this topic [26]. His most recent book, co-authored by Chandler Marrs PhD, is “Thiamine Deficiency Disease, Dysautonomia & High Calorie Malnutrition” and comes highly recommended for anyone seeking to learn more about thiamine deficiency and its importance in our modern world.
References
1. Pekovich SR, Martin PR, Singleton CK. Thiamine Deficiency Decreases Steady-State Transketolase and Pyruvate Dehydrogenase but not α-Ketoglutarate Dehydrogenase mRNA Levels in Three Human Cell Types. The Journal of Nutrition [Internet]. 1998 Apr [cited 2020 Apr 15];128(4):683–7. Available from: https://academic.oup.com/jn/article/128/4/683/4728869
2. SHI Q, KARUPPAGOUNDER S, XU H, PECHMAN D, CHEN H, GIBSON G. Responses of the mitochondrial alpha-ketoglutarate dehydrogenase complex to thiamine deficiency may contribute to regional selective vulnerability. Neurochemistry International [Internet]. 2007 Jun [cited 2020 Apr 15];50(7–8):921–31. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2753422
3. Casteels M, Sniekers M, Fraccascia P, Mannaerts GP, Van Veldhoven PP. The role of 2-hydroxyacyl-CoA lyase, a thiamin pyrophosphate-dependent enzyme, in the peroxisomal metabolism of 3-methyl-branched fatty acids and 2-hydroxy straight-chain fatty acids. Biochemical Society Transactions [Internet]. 2007 Oct 25 [cited 2020 Apr 15];35(5):876–80. Available from: https://pubmed.ncbi.nlm.nih.gov/17956236
4. Elsas LJ, Danner DJ. THE ROLE OF THIAMIN IN MAPLE SYRUP URINE DISEASE. Annals of the New York Academy of Sciences [Internet]. 1982 Mar [cited 2020 Apr 15];378(1 Thiamin):404–21. Available from: https://nyaspubs.onlinelibrary.wiley.com/doi/abs/10.1111/j.1749-6632.1982.tb31214.x
5. Fattal-Valevski A. Thiamine (Vitamin B1). Journal of Evidence-Based Complementary & Alternative Medicine. 2011 Jan;16(1):12–20.
6. Mkrtchyan G, Aleshin V, Parkhomenko Y, Kaehne T, Luigi Di Salvo M, Parroni A, et al. Molecular mechanisms of the non-coenzyme action of thiamin in brain: biochemical, structural and pathway analysis. Scientific Reports [Internet]. 2015 Jul 27 [cited 2020 Apr 15];5(1). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4515825
7. Matthews CC, Zielke HR, Wollack JB, Fishman PS. Enzymatic Degradation Protects Neurons from Glutamate Excitotoxicity. Journal of Neurochemistry [Internet]. 2002 Jan 4 [cited 2020 Apr 15];75(3):1045–52. Available from: https://pubmed.ncbi.nlm.nih.gov/10936185
8. Dhir S, Tarasenko M, Napoli E, Giulivi C. Neurological, Psychiatric, and Biochemical Aspects of Thiamine Deficiency in Children and Adults. Frontiers in Psychiatry [Internet]. 2019 Apr 4 [cited 2020 Apr 15];10. Available from: https://www.frontiersin.org/articles/10.3389/fpsyt.2019.00207/full
9. Shible AA, Ramadurai D, Gergen D, Reynolds PM. Dry Beriberi Due to Thiamine Deficiency Associated with Peripheral Neuropathy and Wernicke’s Encephalopathy Mimicking Guillain-Barré syndrome: A Case Report and Review of the Literature. American Journal of Case Reports [Internet]. 2019 Mar 13 [cited 2020 Apr 15];20:330–4. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6429982
10. Jankowska-Kulawy A, Bielarczyk H, Pawełczyk T, Wróblewska M, Szutowicz A. Acetyl-CoA and acetylcholine metabolism in nerve terminal compartment of thiamine deficient rat brain. Journal of Neurochemistry [Internet]. 2010 Aug 25 [cited 2020 Apr 15];115(2):333–42. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/j.1471-4159.2010.06919.x
11. Nardone R, Höller Y, Storti M, Christova M, Tezzon F, Golaszewski S, et al. Thiamine Deficiency Induced Neurochemical, Neuroanatomical, and Neuropsychological Alterations: A Reappraisal. The Scientific World Journal [Internet]. 2013 [cited 2020 Apr 15];2013:1–8. Available from: https://www.hindawi.com/journals/tswj/2013/309143
12. Hazell AS, Butterworth RF, Hakim AM. Cerebral Vulnerability Is Associated with Selective Increase in Extracellular Glutamate Concentration in Experimental Thiamine Deficiency. Journal of Neurochemistry [Internet]. 1993 Sep [cited 2020 Apr 15];61(3):1155–8. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1471-4159.1993.tb03635.x
13. Bettendorff L. A non-cofactor role of thiamine derivatives in excitable cells? Archives of Physiology and Biochemistry [Internet]. 1996 Jan [cited 2020 Apr 15];104(6):745–51. Available from: https://pubmed.ncbi.nlm.nih.gov/8980789
14. Yamashita H, Zhang Y-X, Nakamura S. The effects of thiamin and its phosphate esters on dopamine release in the rat striatum. Neuroscience Letters [Internet]. 1993 Aug [cited 2020 Apr 15];158(2):229–31. Available from: https://pubmed.ncbi.nlm.nih.gov/8233101
15. Martin PR, Singleton CK, Hiller–Sturmhöfel S. The Role of Thiamine Deficiency in Alcoholic Brain Disease [Internet]. National Institute on Alcohol Abuse and Alcoholism. 2003 [cited 2020 Apr 15]. Available from: https://pubs.niaaa.nih.gov/publications/arh27-2/134-142.htm
16. Lonsdale D. Dysautonomia, a Heuristic Approach to a Revised Model for Etiology of Disease. Evidence-Based Complementary and Alternative Medicine [Internet]. 2009 [cited 2020 Apr 15];6(1):3–10. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2644268
17. Lonsdale D. The Role of Thiamin in High Calorie Malnutrition [Internet]. 2015 [cited 2020 Apr 15]. Available from: https://www.semanticscholar.org/paper/The-Role-of-Thiamin-in-High-Calorie-Malnutrition-Lonsdale/8997c5dc5ba0e0433c04b055c5d55befdc1a8d51
18. Lockman PR, Mumper RJ, Allen DD. Evaluation of blood-brain barrier thiamine efflux using the in situ rat brain perfusion method. Journal of Neurochemistry [Internet]. 2003 Jul 4 [cited 2020 Apr 16];86(3):627–34. Available from: https://onlinelibrary.wiley.com/doi/10.1046/j.1471-4159.2003.01888.x
19. Brown G. Defects of thiamine transport and metabolism. Journal of Inherited Metabolic Disease [Internet]. 2014 May 1 [cited 2020 Apr 16];37(4):577–85. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1007/s10545-014-9712-9
20. Park W-S, Lee J, Hong T, Park G, Youn S, Seo Y, et al. Comparative Pharmacokinetic Analysis of Thiamine and Its Phosphorylated Metabolites Administered as Multivitamin Preparations. Clinical Therapeutics [Internet]. 2016 Oct [cited 2020 Apr 16];38(10):2277–85. Available from: https://pubmed.ncbi.nlm.nih.gov/27707509
21. Nozaki S, Mizuma H, Tanaka M, Jin G, Tahara T, Mizuno K, et al. Thiamine tetrahydrofurfuryl disulfide improves energy metabolism and physical performance during physical-fatigue loading in rats. Nutrition Research [Internet]. 2009 Dec [cited 2020 Apr 16];29(12):867–72. Available from: https://pubmed.ncbi.nlm.nih.gov/19963160
22. Huang W-C, Huang H-Y, Hsu Y-J, Su W-H, Shen S-Y, Lee M-C, et al. The Effects of Thiamine Tetrahydrofurfuryl Disulfide on Physiological Adaption and Exercise Performance Improvement. Nutrients [Internet]. 2018 Jun 29 [cited 2020 Apr 16];10(7):851. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6073388
23. MATSUI K, NAKAHARA H, WATANABE H, TAMATSU H, NAKAZAWA M, NAKAGAWA Y, et al. Inhibition by thiamine tetrahydrofurfuryl disulfide (TTFD) of the arachidonic acid cascade-line activation as evidenced in the heart-lung preparation of the dog. The Japanese Journal of Pharmacology [Internet]. 1985 [cited 2020 Apr 16];39(3):375–9. Available from: https://www.sciencedirect.com/science/article/pii/S0021519819522259
24. Hills JI, Golub MS, Bettendorff L, Keen CL. The effect of thiamin tetrahydrofurfuryl disulfide on behavior of juvenile DBA/2J mice. Neurotoxicology and Teratology [Internet]. 2012 Mar [cited 2020 Apr 16];34(2):242–52. Available from: https://pubmed.ncbi.nlm.nih.gov/21816221
25. Lonsdale D. Thiamine tetrahydrofurfuryl disulfide: A little known therapeutic agent [Internet]. ResearchGate. unknown; 2004 [cited 2020 Apr 16]. Available from: https://www.researchgate.net/publication/8382703_Thiamine_tetrahydrofurfuryl_disulfide_A_little_known_therapeutic_agent
26. Lonsdale D. Publications [Internet]. ResearchGate. ResearchGate; 2020 [cited 2020 Apr 16]. Available from: https://www.researchgate.net/profile/Derrick_Lonsdale2
